Spinal Stenosis is a general term denoting narrowing of the spinal canal, lateral nerve canal (lateral recess), or intervertebral foramina in the lumbar area.
Stenosis often leads to nerve root compression and compromise.
Lumbar spinal stenosis usually develops gradually over time and is widely recognized as a significant source of disability. It is the most common diagnosis associated with lumbar spine surgery in patients older than sixty-five years of age.
The etiology of spinal stenosis may be congenital, acquired or a combination of both these factors. As many as 90% of reported cases of are acquired, resulting from degenerative changes that affect the boney and soft tissues structures of the spinal canal and neighboring intervertebral foramina.
Facet joint degeneration/arthritic changes, thickening of the ligaments in the spinal canal, bulging of the intervertebral discs, spondylolisthesis, post-surgical scarring or any combinations of these conditions may cause spinal stenosis. Other less frequent causes of acquired stenosis include fractures, tumors, infection, or systemic bone diseases such as Paget’s disease.
Causes
Pressure on the nerves can be caused by gradual degenerative changes about the spine with aging.
Arthritis may lead to bone spurs and degenerative changes of the spinal joints (named the facet joints) that result in narrowing of the spinal canal or the foramen where the nerves exit the canal.
Intervertebral disc degeneration, herniation or bulging, as well as thickening of ligaments within the spinal canal may lead to increased pressure on the nerves as well.
Less frequently, synovial, meningeal or other spinal tumors may cause narrowing of spinal structures as well.
Symptoms
Patients with lumbar spinal stenosis typically present with an extended history of
- low back pain
- progressive leg discomfort
Unilateral or bilateral leg symptoms occur in approximately 90% of stenosis patients and is often referred to as neurogenic claudication.
Neurogenic claudication is defined as poorly localized pain, tingling, or cramping in one or both legs that is believed to result from compression of the neural elements (nerves and associated membranes) of the lumbar spine.
Symptoms are typically posture-dependent, worsening with walking or weight-bearing.
Patients report mounting discomfort with walking and standing which is quickly relieved by sitting or adopting a flexed forward posture.
Classification of spinal stenosis based on pathologic anatomy provides the treating clinician with information essential to the design and implementation of an appropriate treatment plan; however, poor correlation exists between the severity of patient symptoms and imaging study findings.
The formulation of an effective treatment plan relies on the integration of imaging and other studies with the patient’s clinical signs and symptoms.
Diagnosis
The diagnosis of spinal stenosis begins with a complete history and physical examination. The doctor will determine what symptoms are present, what makes them better or worse, and how long they have been present. A physical examination is essential for determining how severe the condition is, and whether or not it is causing pain, weakness or numbness.
Abnormalities in the strength and sensation of particular parts of the body that are found with a neurological examination may provide objective evidence of chronic nerve root compression caused by spinal stenosis.
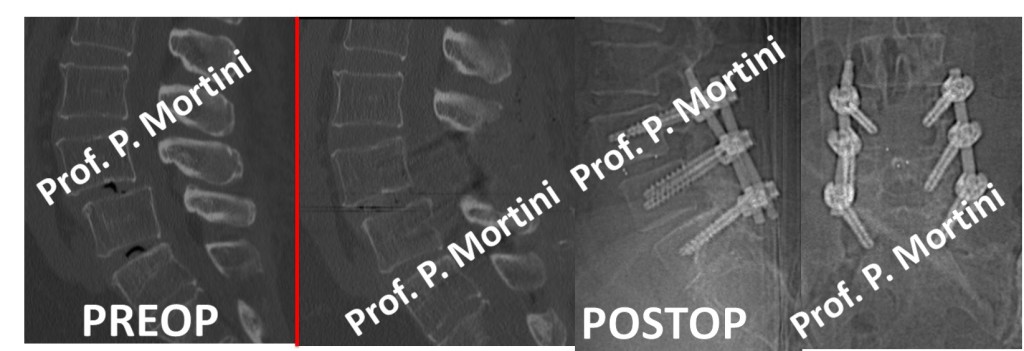
Radiographs (X-rays), CT scans (CAT scan), Magnetic Resonance Imaging (MRIs) or electromyographic tests (EMGs) may be conducted to assist in evaluating whether spinal stenosis is present.
Treatment
For treatment, the initial conservative approach is often physical therapy; most back problems respond to non-surgical treatments. Non-surgical treatments may include anti-inflammatory medication, physical therapy or pain management techniques such as epidural spinal injections.
Patient education on proper posture and improved mobility plays an important part in the rehabilitation of spinal stenosis patients.
When conservative treatments don’t help, surgery often provides relief. For patients with persistent pain, a decompressive lumbar laminectomy (or other procedures) may be recommended to remove portions of the damaged bone, joints, disc or ligaments that are pressing on nerve roots. Most post-surgical patients leave the hospital after a brief stay.
 English
English Italiano
Italiano